
Devices/Diagnostics: Emergency Use Authorizations During the COVID-19 Pandemic
In this blog post, Michelle O’Connor, senior director of regulatory affairs, and Ken Butz, associate director of regulatory affairs, discuss the increased uptake of Emergency Use Authorizations (EUAs) for medical devices during the COVID-19 pandemic.
EUAs for MedTech Increase
While EUAs for therapeutics and vaccines have garnered a great deal of visibility during the pandemic, we’ve also seen a remarkable rise in the number of MedTech products specifically related to SARS-CoV-2 (COVID-19) being considered for emergency use. In fact, the U.S. Food and Drug Administration is now receiving 40 EUA submissions per week [1], making a thorough and complete application critical to an efficient and successful review.
As background, Section 564(b) of the U.S. Food, Drug & Cosmetic (FD&C) Act (public health emergency declaration) enables the FDA to issue EUAs, which facilitate the emergency use of an unapproved drug, uncleared device, unlicensed biological product or an unapproved use of any of these by reviewing available data under an expedited pathway detailed in FDA Guidance on the Emergency Use Authorization of Medical Products and Related Authorities.
This guidance also details the content of an EUA submission, including a description of the product and its intended use, the need for the product, safety and effectiveness data, a discussion of risks and benefits, and information equivalent to a package insert or instructions for use. Importantly, the EUA provides evidence that the product may be effective, in advance of establishing reasonable assurance that the product is safe and effective, which is required for a full marketing authorization.[2] Tests are expected to follow the 510(k) pathway after the initial test reviewed receives a de novo reclassification.
There is an extensive list of medical devices that could be used for the management of COVID-19 for which an EUA route is available. These include:
- In-Vitro Diagnostics
- Serology/antibody tests
- Tests for management of COVID-19 patients
- Personal protective equipment
- Blood purification devices
- Continuous renal replacement therapy and hemodialysis devices
- Decontamination systems for Personal Protective Equipment
- Infusion pumps
- Remote or wearable patient monitoring devices
- Respiratory assist devices
- Ventilator and ventilator accessories
- Other – e.g., catheters, face masks
According to a report in Global Data,[3] devices have seen a recent surge in sales based on an overwhelming demand for solutions in the management of the pandemic.
FDA Focus on Diagnostics and Related Guidance
With the emphasis on more reliable and convenient testing, there has been intense development to address this unmet need in COVID-19 diagnostics. Testing plays an essential role in screening and monitoring of COVID-19 infection, including emerging variant strains of SARS-CoV-2. Specifically, FDA is focusing on three different types of In Vitro Diagnostic (IVD) tests:
- Diagnostic tests: tests that detect parts of the SARS-CoV-2 virus and can be used to diagnose infection with the SARS-CoV-2 virus, including both molecular tests and antigen tests.
- Serology/Antibody tests: tests that detect antibodies (e.g., immunoglobulin M, immunoglobulin G) to the SARS-CoV-2 virus.
- Tests for management of COVID-19 patients: tests that are used in the management of patients with COVID-19, such as tests to detect biomarkers related to inflammation.
FDA developed guidance, Policy for Coronavirus Disease-2019 Tests During the Public Health Emergency (Revised 11 May 2020), with a series of published EUA templates to facilitate interactions with the agency and applications.
The agency has been proactive in providing guidance, holding weekly virtual town hall meetings to respond to questions from commercial test developers and ensure understanding in a rapidly evolving regulatory environment. In February 2021, FDA issued a new guidance for test developers on the potential impact of emerging and future viral mutations of SARS-CoV-2 on COVID-19 tests (Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests), recognizing that the presence of SARS-CoV-2 mutations in the SARS-CoV-2 virus in a patient sample can potentially change the performance of a test. FDA recommends that developers design their test to minimize the impact of viral mutations on test performance, routinely monitor for viral mutations that may impact the test performance and provide clarity on limitations of the test on the diagnostic labeling.
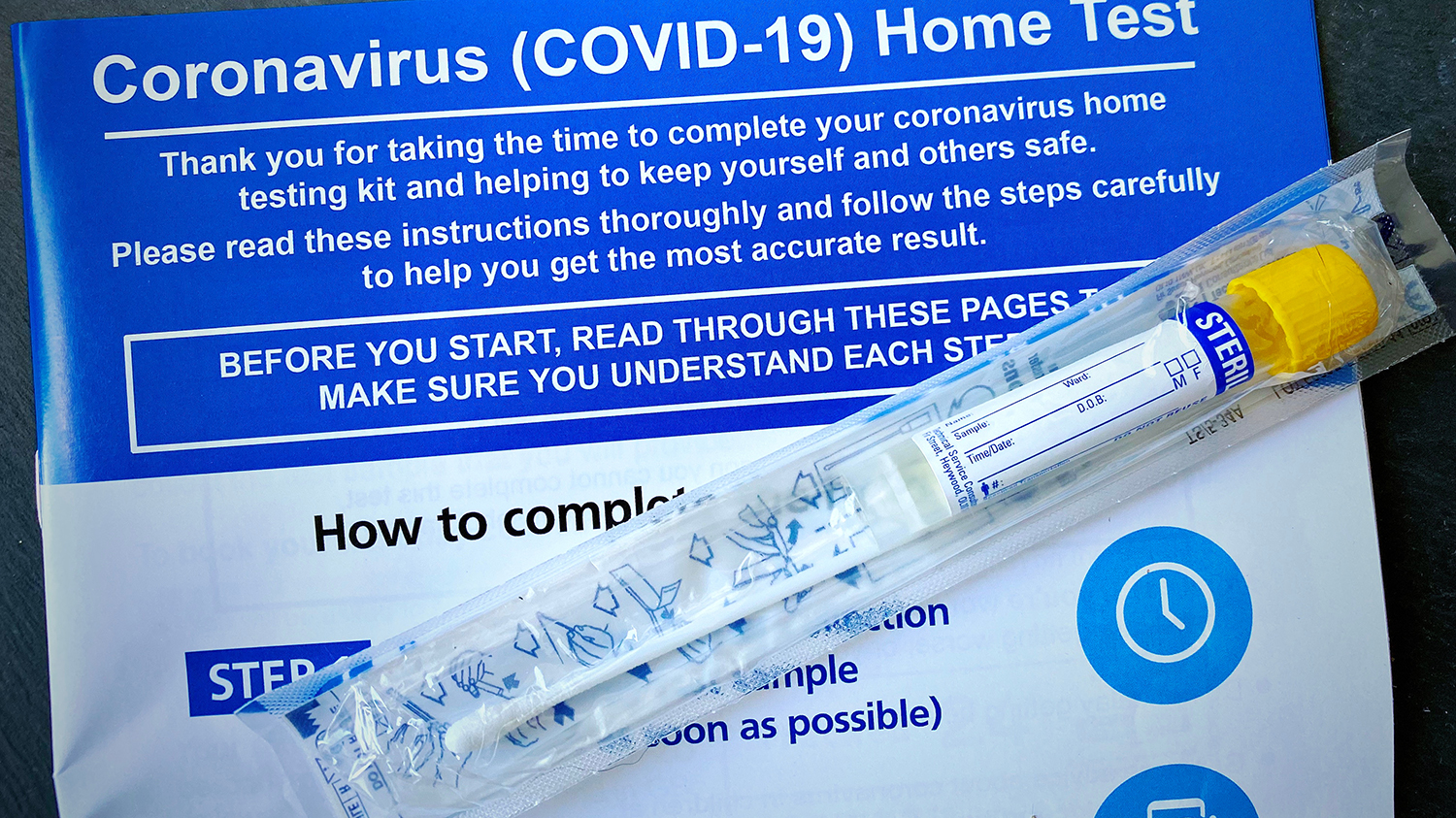
As of 16 March 2021, FDA had granted EUAs for 327 tests and sample collection devices including 254 molecular tests, 72 antibody tests and 15 antigen tests. Thirty-eight molecular tests are authorized that can be used with home-collected samples. Of note, only five tests have been authorized for at-home use – one molecular prescription at-home test, two antigen prescription at-home tests, one over-the-counter (OTC) at-home antigen test, and one OTC molecular test. To address this unmet need, the FDA is now focusing on a subset of test formats: non-laboratory or at-home tests, tests used in a point-of-care environment and high-throughput laboratory tests.
A pre-EUA engagement is often required to align with the agency on the overall development plan and test or technology-specific requirements. For a pre-EUA, the template form may be completed with the available information. It is important to address the analytic studies early in the process, considering the current shortage of laboratory testing bandwidth and materials. Specific agreement on the appropriate study design, including the authorized comparator for assessing the positive predictive agreement of the test, is important. Additional discussions pertaining to software or mobile apps (if applicable), and post-authorization requirements, are also valuable.
Recent Observations
PPD has supported a number of EUAs for COVID-19 diagnostics. Successful EUA applications must include complete information and supporting data that address the published FDA interactive review templates including well-organized clinical and analytical study reports. Pertinent aspects that lead to a successful application include:
- All assays should demonstrate high analytical sensitivity as determined by testing with the FDA SARS-CoV-2 Reference Panel; comparative results are posted on the FDA website. Specimens tested should be thoroughly characterized including storage duration and conditions, stability information and a description of how specimens were tested. External positive and negative control materials should be validated within analytical and clinical studies.
- Well-designed clinical studies with inclusion and exclusion criteria for patient enrollment supportive of the intended use and proposed claims are essential. With rapidly changing COVID-19 prevalence maps, appropriate study designs and operations are needed to align with the intended use of the test and to ensure test performance over a full range of viral loads. Additionally, at-home tests require human factors or usability studies that can be designed and conducted by PPD.
- Product labeling and compliant reporting requirements are key components and include a package insert, instructions for use, or quick reference guide and “fact sheets” to be furnished to health care professionals and recipients of the product. For non-laboratory or tests performed at home, a method for reporting results to healthcare professionals and relevant public health authorities is required.
Surveillance Needs Beyond Issuance of the EUA
Highly sensitive SARS-CoV-2 diagnostic tests are essential for rapidly identifying COVID-19 infections thereby containing spread and preventing deaths. An EUA is an effective tool in accelerating the development and marketing of critical tests. Importantly, test development does not end with issuance of the EUA. With new mutations and variants emerging, test developers along with FDA have an essential role in ongoing surveillance to evaluate the impact of new variants and ensure ongoing effective test performance. Development and implementation of effective diagnostic testing strategies play a key role along with vaccines and therapeutics in managing the current pandemic as well as preparing for future health needs.
For further information on this topic please contact our Regulatory Intelligence Policy and Advocacy Team at